Why those most at risk of COVID-19 are least likely to respond to a vaccine
Aging immune systems spell trouble for any vaccine candidate, but there are ways to overcome this hurdle.
If you want to pinpoint an organ that’s key to fighting COVID-19—and to understanding why the disease is so hard on older people—point your finger at the middle of your chest and run it up along your sternum. Stop just before you reach your neckline. Right there, nestled just behind the bone in between the lungs, is the gland that captivated Edith Boyd’s curiosity in the 1930s: the thymus.
Boyd set out to understand how aging affects its size. She combed through data from 10,000 autopsies collected at the University of Minnesota, where she was an assistant professor, and analyzed information gathered by scientists from four European countries too. She confirmed an interesting pattern: The thymus, about the size of a pack of Wrigley’s chewing gum in infants, seemed to get bigger through puberty—then shrank steadily after that.
Another 30 years went by before scientists figured out the thymus’s purpose; it was the last major organ to have its function found. It turned out to be the source of T-cells, a major set of pathogen fighters, some of which also help the immune system make additional defenses such as antibodies.
That discovery combined with insights from anatomists like Boyd ultimately reveal why emerging infectious diseases like COVID-19 can be a double-whammy for older adults. Firstly, aging depletes the arsenal of adaptable T-cells, as the thymus fills with fatty tissue. As a result, our immune systems become ill-equipped to fight off new viruses. A July 17 analysis of more than 50,000 coronavirus deaths in the U.S. found that 80 percent were people 65 or older.
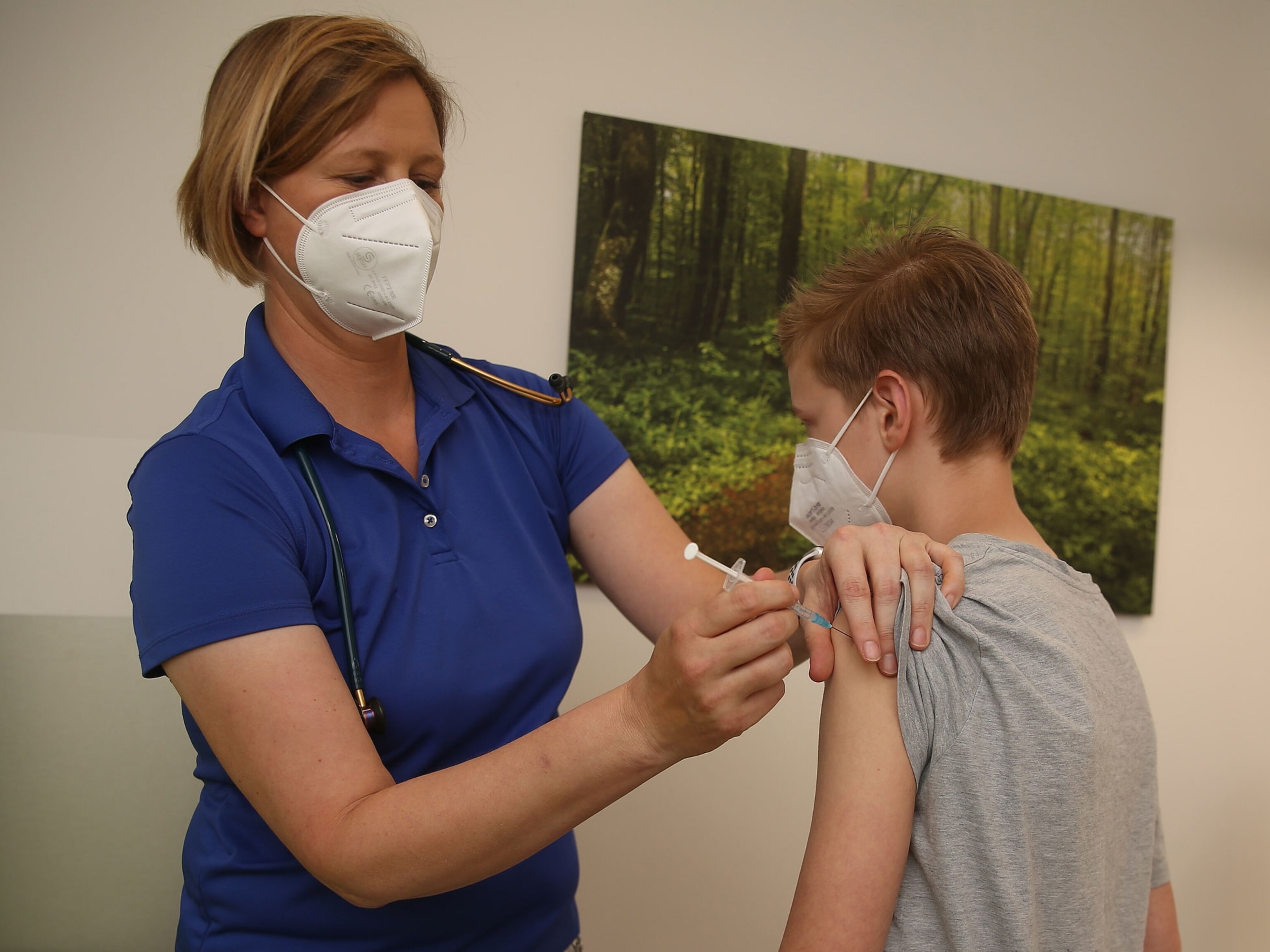
Because of COVID-19, researchers are having to pay more attention than ever to how vaccines perform in older people.
Second, the aging thymus may also complicate vaccine development for the pandemic. Vaccines provide instructions for our immune system, which T-cells help pass along. By age 40 or 50, the thymus has exhausted most of its reserve of the kind of T-cells that can learn to recognize unfamiliar pathogens—and ‘train’ other immune cells to fight them. Many vaccines rely on such T-cells.
Because of COVID-19, researchers are having to pay more attention than ever to how vaccines perform in older people. Moderna Therapeutics, for example, which published the first results this week from the phase-one trial of its novel mRNA vaccine, is running a phase two trial specifically for adults aged 55 and older.
“Up until very recently most of the focus of the vaccine community has been on saving lives of young children,” says Martin Friede, the World Health Organization’s coordinator for vaccine product and delivery research. “The people who need the vaccine the most may actually be the people in whom the vaccine might not work.”
Trials in older individuals are also crucial because not everyone ages in the same way, Friede adds. It’s not just about the thymus: Some people might be jaunting off to the golf course whereas others are too frail to walk—and these differences in individual vitality might translate into different vaccine responses.
Drug developers can tweak their vaccines to increase the odds that older people will be protected. But making these modifications—and getting vaccine doubters to accept them—can be tricky.
Stimulating aged immunity
Vaccine makers have gained some experience with “immunosenescence”—the dysfunction of the aging immune system—in dealing with influenza. Older people are more susceptible to it, and flu vaccines typically protect them less.
To overcome that, vaccine giant Sanofi Pasteur, for example, created an influenza vaccine called Fluzone for people 65 and older that contains four times as much immune-stimulating ‘antigen’, a molecular component of a pathogen that can trigger the body to make protective antibodies. A 2014 study found that the high-dose version was 24 percent more effective than the regular dose.
Another way to boost the efficacy of flu immunizations for older people is to use adjuvants—added ingredients that make vaccines stimulate the immune system more strongly. The Fluad vaccine, for instance, contains the adjuvant MF59, which is partially derived from squalene, a natural oil produced by the skin and by plants.
Adjuvants have been used for around a century in vaccines, not just for flu or for older people. But even tried-and-tested ones have been framed as dangerous by anti-vaccine crusaders.
For example, a squalene-based adjuvant called AS03 from the pharmaceutical company GSK was used in a vaccine deployed against the 2009 swine flu pandemic. The vaccine was withdrawn from the market after reports of narcolepsy emerged in Scandinavia, and it was never on the market in the United States. A 2014 study with 1.5 million people conducted by the Centers for Disease Control and Prevention found no connection between the pandemic vaccine and narcolepsy—but anti-vaccine groups have continued to blame the adjuvant, pushing the notion that it elicited excessive immune reactions.
Doctors worry that such misinformation about adjuvants might cause people to hesitate to get immunized with a COVID-19 vaccine.
“Anti-vaxxers are looking for any reason to deny a vaccine,” says Wilbur Chen, who directs adult clinical studies at the University of Maryland’s Center for Vaccine Development and Global Health. “The discussion for them now is, ‘Oh, these adjuvants are dangerous,’” he adds.
But Chen cautions vaccine developers against acquiescing to this: “The problem when we do address their concern is that it inadvertently gives legitimacy to their concern, and then they say, ‘Ah well, you see it was a real concern and that’s why they changed it.’”
GSK has said it will produce large volumes of the AS03 adjuvant for potential use by partners developing multiple COVID-19 vaccines. The company says that the narcolepsy experienced by some people after receiving the swine flu vaccine was triggered by a reaction to the H1N1 flu virus itself that was circulating in the population.
What’s old is not new
Old age does not always determine the outcome of COVID-19. News headlines tell of centenarians beating the disease and of teens dying from it. A new paper in the journal Science documents a range of immune responses to COVID-19, independent of age, including one that was essentially a non-response.
That lack of response among some older people in the study “could be linked to immunosenescence,” speculates Michael Betts, an immunologist at the University of Pennsylvania’s Perelman School of Medicine and an author of the study. “Some people will do better than others, and right now we don’t necessarily know the drivers of that.”
Immunosenescence isn’t only a depletion of certain T- cells. It also weakens the ‘innate’ immune response, the frontline defense the body mounts against invading microbes, even before making antibodies that can recognize a specific antigen.
To make matters worse, immunosenescence isn’t the only challenge facing researchers trying to design COVID-19 vaccines for older people. There’s increasing evidence that many elders have another problem: their immune system is preoccupied with fighting viruses that cause lifelong infections once they enter the body, such as the typically benign cytomegalovirus (CMV).
“When you look at the elderly, 20 percent of the immune system is sometimes directed toward CMV,” says David Kaslow, vice president for essential medicines at PATH, a Seattle non-profit. “Suppressing all these viruses comes at a cost.”
Scientists call it “inflammaging”: the immune system is essentially stuck in an inflammatory state. That might make it harder for the body to detect a new pathogen like COVID-19—or to get stimulated by a vaccine against it.
“It’s essentially like being in a room with lots of noise and someone says help,” Friede explains. “You won’t hear it.”
Researchers trying to study these problems of immune aging in the lab face a peculiar problem: a shortage of old mice. Maintaining older mice is expensive for suppliers, so they don’t usually keep a large stock.
“I tried to place an order for the old mice late last week with our usual supplier,” says Byram Bridle, a viral immunologist at the University of Guelph’s Ontario Veterinary College in Canada. “They have no old mice and have just recently started a program to allow some mice to age. They will not have mice that are 18 months old available for research until January 2021.”
Finally, vaccine researchers face the fundamental problem of COVID-19: None of us have encountered the new coronavirus before. Other vaccines that have been tailored to older people, including those against flu and shingles, are essentially booster shots, according to Friede, because everyone has been exposed to influenza and most older people have had chickenpox, the virus that also causes shingles.
Moreover, because of exposure to a lifetime of cold-causing coronaviruses, seniors may already have a repertoire of antibodies that glom onto SARS-CoV-2, the virus that causes COVID-19. That could counterintuitively hamper the body from designing better antibodies against it. “It might actually be bad for infection,” Betts says.
Or, past infections by such germs could be a good thing. There’s new evidence that exposure to the 2003 SARS outbreak or coronaviruses from animals has equipped some people with a T-cell response against SARS-CoV-2. Broader study is required to determine the extent of this protection and what it might mean for a vaccine, given the virus may still be completely novel to many immune systems.
“For COVID-19, we are likely going to have to prime the population against something that they’ve never seen before,” Friede says.
Related Topics
You May Also Like
Go Further
Animals
- Soy, skim … spider. Are any of these technically milk?Soy, skim … spider. Are any of these technically milk?
- This pristine piece of the Amazon shows nature’s resilienceThis pristine piece of the Amazon shows nature’s resilience
- Octopuses have a lot of secrets. Can you guess 8 of them?
- Animals
- Feature
Octopuses have a lot of secrets. Can you guess 8 of them? - This biologist and her rescue dog help protect bears in the AndesThis biologist and her rescue dog help protect bears in the Andes
Environment
- This pristine piece of the Amazon shows nature’s resilienceThis pristine piece of the Amazon shows nature’s resilience
- Listen to 30 years of climate change transformed into haunting musicListen to 30 years of climate change transformed into haunting music
- This ancient society tried to stop El Niño—with child sacrificeThis ancient society tried to stop El Niño—with child sacrifice
- U.S. plans to clean its drinking water. What does that mean?U.S. plans to clean its drinking water. What does that mean?
History & Culture
- Beauty is pain—at least it was in 17th-century SpainBeauty is pain—at least it was in 17th-century Spain
- The real spies who inspired ‘The Ministry of Ungentlemanly Warfare’The real spies who inspired ‘The Ministry of Ungentlemanly Warfare’
- Heard of Zoroastrianism? The religion still has fervent followersHeard of Zoroastrianism? The religion still has fervent followers
- Strange clues in a Maya temple reveal a fiery political dramaStrange clues in a Maya temple reveal a fiery political drama
- How technology is revealing secrets in these ancient scrollsHow technology is revealing secrets in these ancient scrolls
Science
- Soy, skim … spider. Are any of these technically milk?Soy, skim … spider. Are any of these technically milk?
- Can aspirin help protect against colorectal cancers?Can aspirin help protect against colorectal cancers?
- The unexpected health benefits of Ozempic and MounjaroThe unexpected health benefits of Ozempic and Mounjaro
- Do you have an inner monologue? Here’s what it reveals about you.Do you have an inner monologue? Here’s what it reveals about you.
- Jupiter’s volcanic moon Io has been erupting for billions of yearsJupiter’s volcanic moon Io has been erupting for billions of years
Travel
- Follow in the footsteps of Robin Hood in Sherwood ForestFollow in the footsteps of Robin Hood in Sherwood Forest
- This chef is taking Indian cuisine in a bold new directionThis chef is taking Indian cuisine in a bold new direction
- On the path of Latin America's greatest wildlife migrationOn the path of Latin America's greatest wildlife migration
- Everything you need to know about Everglades National ParkEverything you need to know about Everglades National Park