Microbes in your gut may be new recruits in the fight against viruses
Microbiologists are looking at new ways to fight viral infections, including COVID-19, with the bacteria already living in your intestine.

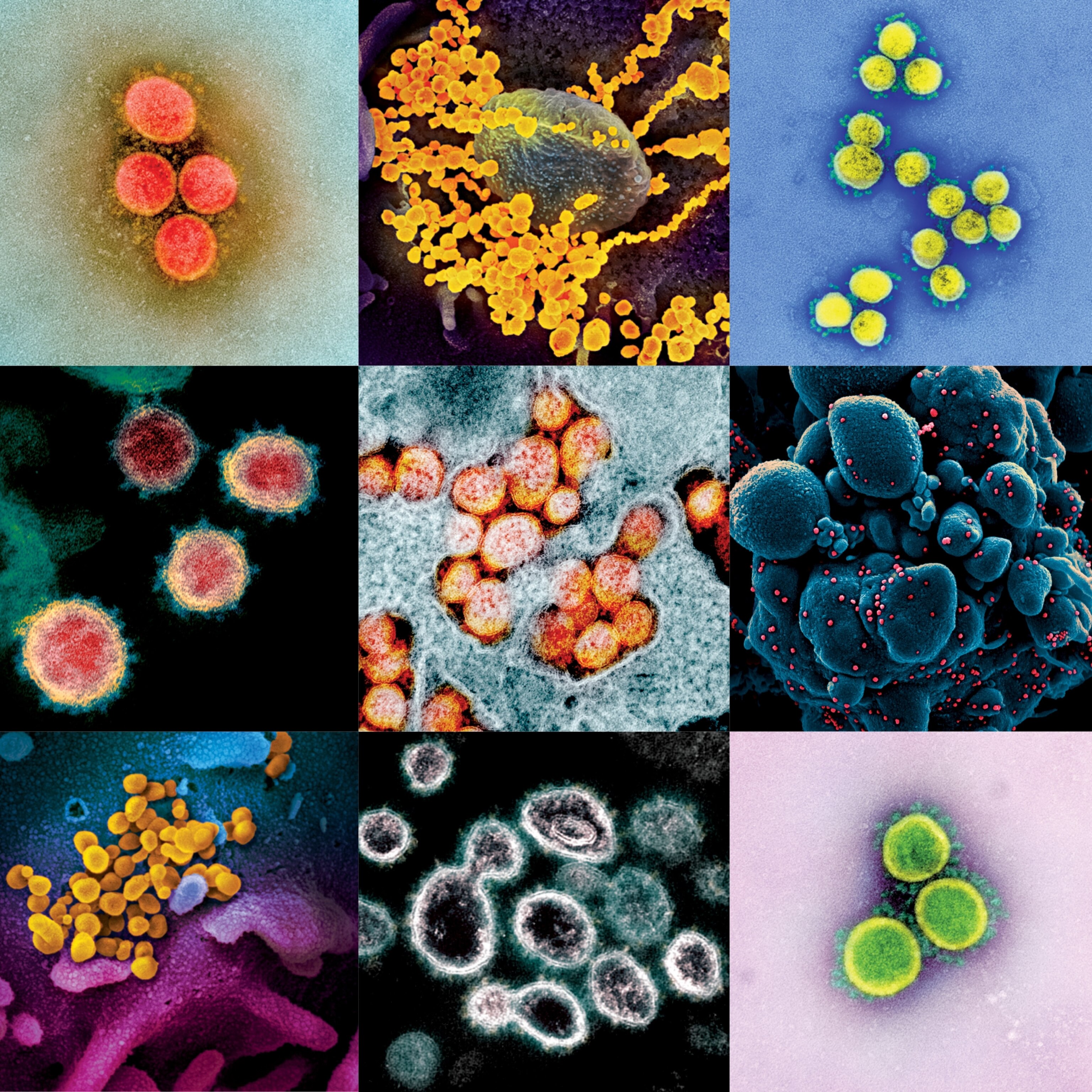
The parasitic lifestyle of viruses makes them a challenging nemesis. Traditional lines of defense, such as antiviral drugs and vaccines, are difficult to develop, can produce undesirable side effects, and may lose efficacy if the virus mutates. Some scientists are now thinking outside the box, pointing out that we’re not alone in this fight. Trillions of microbes living in and on us—collectively known as the human microbiome—call the body home and need it to survive. Today researchers are testing whether they can draft these microbes into the immune system’s army to help fight viral invaders.
In the past few decades, scientists have learned a great deal about the gut microbiome, particularly the bacterial component. It has been well established that intestinal bacteria assist with digestion and make certain nutrients. They also appear to communicate with other parts of the body such as the brain using chemical signals. For example, intestinal bacteria make neurotransmitters like serotonin that may regulate mood or mental states. They can also affect the immune system, which has captured the attention of infectious disease researchers.
“Imagine microbes that block a virus from entering a cell or communicate with the cell and make it a less desirable place for the virus to set up residence,” says Mark Kaplan, chair of the department of microbiology and immunology at the Indiana University School of Medicine. “Manipulating those lines of communication might give us an arsenal to help your body fight the virus more effectively.”
The scourge of COVID-19, caused by the virus SARS-CoV-2, has heightened interest in the potential connection between a person’s microbiome and their ability to fight a viral infection. COVID-19 produces few to no symptoms in many people but can become life-threatening in others. What drives these dramatically different responses to SARS-CoV-2 infection remains a mystery, but new studies are suggesting that the state of the patient’s microbiome may be a contributing factor.
COVID-19 is usually worse in the elderly, as well as people of any age with preexisting conditions such as obesity, diabetes, and cancer. These preexisting medical conditions have also been linked to differences in a person’s microbiome. And a number of preliminary studies have documented unusual microbiomes in hospitalized COVID-19 patients. If there is a strong connection between gut microbes and COVID-19 severity, it may be possible to alter the microbiome to fight SARS-CoV-2 and other viruses.
“If we consider intestinal bacteria to be the gatekeepers between what we eat and our body,” says Kaplan, “one can appreciate that some gatekeepers might be more effective than others at fighting off intruders.”
How the gut microbiome helps
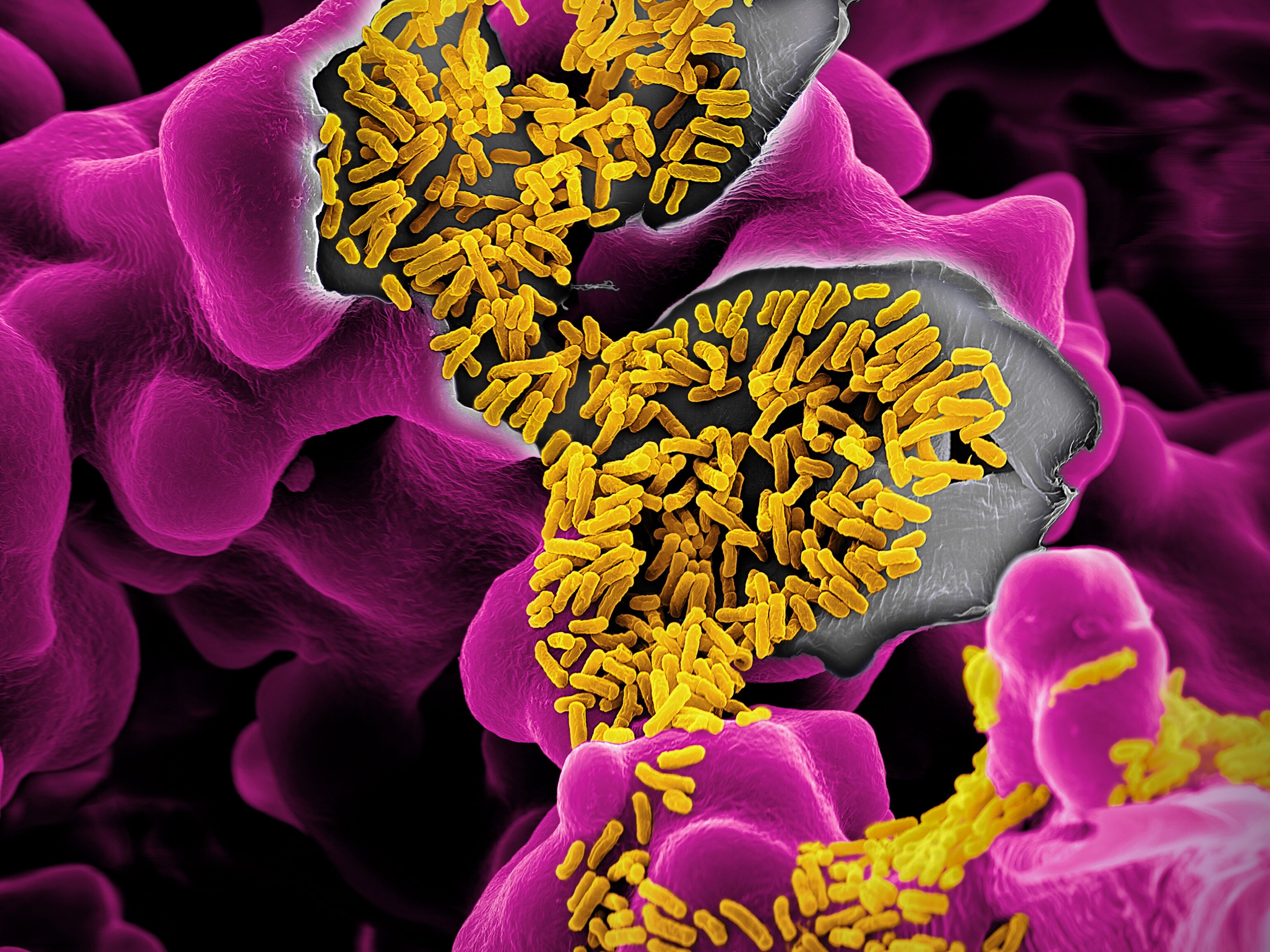
Hundreds of different species of bacteria live in the gut. This community contains an estimated 40 trillion cells, which is slightly more than the number of human cells making up your body. This enormous collective may help ward off viruses through three primary mechanisms: building a wall that blocks invaders, deploying advanced weaponry, and providing support to the immune system.
To understand the first line of defense, remember that your intestine is like a tube. In this tube, food is broken down so that nutrients can be absorbed. At the same time, waste material containing harmful biochemicals is generated, and pathogens that were inadvertently consumed are also present. To keep waste and disease-causing microbes moving to the exit door, the cells of the intestine’s inner wall produce a layer of protective mucus. Intestinal bacteria appear to influence the production of this important mucus barrier, which could prevent viruses in the gut from reaching other parts of the body.
But when this mucus layer is damaged, the gut can leak. This enables waste products and possibly dangerous pathogens to escape into other organ systems, where they can cause detrimental inflammation or infection. “It is highly likely that viruses get access to organs other than the lungs and the gut through a leaky gut,” explains microbiologist Heenam Stanley Kim at Korea University in Seoul.
A leaky gut may also promote autoimmune disease. As such, some scientists have proposed that perturbations in the gut microbiome may be linked to the so-called “cytokine storm,” an overreactive immune response thought to be a potential driver of severe COVID-19.
In addition to the lungs and gut, the SARS-CoV-2 virus has been detected in the liver, kidney, heart, and brain.
Furthermore, evidence is mounting that the microbes in the gut might influence the health of the lungs through chemical communication. In macaques, for example, researchers found that SARS-CoV-2 altered the gut microbiome by the tenth day of infection; with some of the changes persisting after 26 days. Notably, the infected macaques displayed a drop in bacterial species known to make short-chain fatty acids (SCFAs), which are important molecules that can regulate the immune system. Studies in mice have revealed SCFAs produced by gut microbes travel via the bloodstream to other areas of the body, including the lungs, and protect the animals from respiratory viruses.
The microbiome could also battle viruses by producing chemicals that interfere with the viral life cycle. For example, some bacteria produce toxins called bacteriocins to combat other competing strains of bacteria. But studies performed in laboratory cultured cells suggest these bacteriocins may also inhibit the activity of certain viruses. Streptomycetes bacteria manufacture a bacteriocin, called duramycin, that blocks the entry of West Nile, dengue, and Ebola viruses into their host cells. Other bacteriocins halt the replication of herpes simplex viruses.
A third way the microbiome may help fight viruses is through support of the immune system. One trial showed subjects who received Lactobacillus, bacteria commonly found in fermented foods and yogurt, in conjunction with a booster polio vaccination produced polio virus-neutralizing antibodies at a higher rate.
Another study, led by immunologist Dennis Kasper at the Blavatnik Institute at Harvard Medical School, showed that gut bacteria known as Bacteroidetes trigger intestinal immune cells to release interferons. Interferons are key factors that ramp up the body’s response to viruses and help eliminate cells that are infected. When the microbiome becomes abnormal, or dysbiotic, our immune defenses may become compromised. “Bacteroidetes make up about 40 to 50 percent of the 200-plus microbial species in the gut of most of us" Kasper says. "When people are dysbiotic and don’t have this normal balance of microbes, they are more susceptible to various illness.”
“Perhaps in dysbiotic people with lower numbers of these Bacteroidetes in the gut,” Kasper adds, “there is less resistance when encountering a virus and therefore more severe infection.”
Hacking the microbiome
Given the mounting evidence of the microbiome’s role in fortifying the immune system to fight viruses, researchers are exploring how to translate these findings into therapies and diagnostics.
As certain bacterial species in the gut have been linked to worse outcomes during viral infection, some researchers have proposed using these bacteria as “biomarkers,” or diagnostic indicators. For example, microbiologist Ana Maldonado-Contreras at the University of Massachusetts Medical School recently reported in preliminary research that Enterococcus faecalis, gut bacteria also linked to chronic inflammation, is a reliable predictor of severe COVID-19. Maldonado-Contreras says that testing for this bacterial species “might be an efficient means to identify patients who are more likely to develop a severe form of infection that requires greater care and clinical intervention.”
In terms of treatment, researchers have achieved remarkable success in transplanting a healthy microbiome into a patient with an unhealthy one. The procedure is called fecal microbiota transplantation and is currently approved only in the treatment of bacterial colitis cases caused by Clostridium difficile infection (CDI). Fecal microbiota transplantation successfully cures more than 90 percent of patients with CDI, suggesting that other diseases also may be treated using this technique. “If gut health affects COVID-19 prognosis, we should exploit it for better management and prevention of the disease," Kim argues. "I suggest that fecal microbiota transplantation can be carefully considered at least for the patients who have a poor prognosis.”
Another innovative way to alter the microbiome may be through bacteriophages, which are viruses that infect and kill certain species of bacteria. In theory, bacteriophages could be administered to patients to weed out bacterial species from the microbiome that hinder the immune system’s ability to fight viral infections. In other words, a bacteria-targeting virus would be used to fight a virus infecting human cells by altering bacteria living in the human gut.
Rather than reshaping the microbiome, some researchers favor a more refined approach. If the beneficial molecules made by a certain species of gut bacteria could be identified, it is possible they could be manufactured and packaged into a pill.
For example, the Bacteroidetes bacteria, mentioned above, have a specific molecule on their cell surface called a glycolipid that causes intestinal immune cells to release antiviral interferons. “One exciting potential of our finding is that the glycolipid that induces type I interferon can be synthesized and potentially be used prophylactically in individuals at risk,” Kasper says. His team tested this idea and found that mice could be protected from a viral infection by adding this bacterial glycolipid into their drinking water.
How the microbiome interacts with viruses is complex. Most studies have focused on the bacterial branch of our microbiome, leaving the contributions of gut fungi, protozoa, bacteriophages and other viruses largely unexamined. But further research promises to reveal new therapeutic strategies that could be exploited in the battle against infectious diseases.
Cultivating a healthy microbiome
As knowledge of the intestinal microbiome is still in its infancy, some argue that it is premature to draw firm conclusions about its role in fighting viral infections like COVID-19.
Microbiologist Jonathan Eisen, director of the microbiome special research program at the University of California, Davis, cautions that more research is required. "I am concerned about claims regarding a potential causative role of the microbiome in risk for COVID-19 infection and severity without evidence for such a causal role.” To date, only correlations have been observed between COVID-19 infection, inflammation markers, and the microbiome, says Eisen. The challenge is to determine which factor might cause these correlations—they could, for example, be driven by changes in diet that occur when someone gets sick or could be due to immune response to getting infected. “But we cannot at this time conclude that the microbiome has played any direct role in any COVID-related issues.”
It is also difficult to provide precise directives on how to augment the microbiome to resist viral infection. Everyone’s microbiome is different, populated through a complex mix of genetic, dietary, and environmental influences. There is general consensus, however, that a diet rich in prebiotics and probiotics, along with regular exercise, helps promote a healthy microbiome and protects against leaky gut.
Prebiotics are a type of fiber and are only found in plants or certain supplements. Foods high in fiber include artichokes, asparagus, onions, beans, and berries. “Prebiotics have been well studied and have been shown to improve gut integrity,” says medical journalist Scott Anderson, author of The Psychobiotic Revolution. Probiotic foods contain live bacteria or yeast that are beneficial for digestive health; they include fermented foods like kefir, sauerkraut, kimchi, as well as yogurt.
In terms of exercise, studies in mice have shown that exercise lowers inflammation and promotes gut integrity. “Exercise is known to improve SCFA levels by balancing the microbiota, which helps nourish and heal the cells lining the gut,” Anderson adds. That in turn could prevent complications of viral infection caused by a leaky gut.
Kim hopes that these new studies help motivate people to take proper care of their microbes to guard against infection and chronic inflammatory illness. “Increasing fiber in our diet is an effective way to improve the gut microbiome and it may help better management and prevention of COVID-19 now and also of chronic diseases throughout life.”
Related Topics
You May Also Like
Go Further
Animals
- This ‘saber-toothed’ salmon wasn’t quite what we thoughtThis ‘saber-toothed’ salmon wasn’t quite what we thought
- Why this rhino-zebra friendship makes perfect senseWhy this rhino-zebra friendship makes perfect sense
- When did bioluminescence evolve? It’s older than we thought.When did bioluminescence evolve? It’s older than we thought.
- Soy, skim … spider. Are any of these technically milk?Soy, skim … spider. Are any of these technically milk?
- This pristine piece of the Amazon shows nature’s resilienceThis pristine piece of the Amazon shows nature’s resilience
Environment
- This pristine piece of the Amazon shows nature’s resilienceThis pristine piece of the Amazon shows nature’s resilience
- Listen to 30 years of climate change transformed into haunting musicListen to 30 years of climate change transformed into haunting music
- This ancient society tried to stop El Niño—with child sacrificeThis ancient society tried to stop El Niño—with child sacrifice
- U.S. plans to clean its drinking water. What does that mean?U.S. plans to clean its drinking water. What does that mean?
History & Culture
- Meet the original members of the tortured poets departmentMeet the original members of the tortured poets department
- Séances at the White House? Why these first ladies turned to the occultSéances at the White House? Why these first ladies turned to the occult
- Gambling is everywhere now. When is that a problem?Gambling is everywhere now. When is that a problem?
- Beauty is pain—at least it was in 17th-century SpainBeauty is pain—at least it was in 17th-century Spain
- The real spies who inspired ‘The Ministry of Ungentlemanly Warfare’The real spies who inspired ‘The Ministry of Ungentlemanly Warfare’
Science
- Here's how astronomers found one of the rarest phenomenons in spaceHere's how astronomers found one of the rarest phenomenons in space
- Not an extrovert or introvert? There’s a word for that.Not an extrovert or introvert? There’s a word for that.
- NASA has a plan to clean up space junk—but is going green enough?NASA has a plan to clean up space junk—but is going green enough?
- Soy, skim … spider. Are any of these technically milk?Soy, skim … spider. Are any of these technically milk?
- Can aspirin help protect against colorectal cancers?Can aspirin help protect against colorectal cancers?
Travel
- What it's like to hike the Camino del Mayab in MexicoWhat it's like to hike the Camino del Mayab in Mexico
- Is this small English town Yorkshire's culinary capital?Is this small English town Yorkshire's culinary capital?
- This chef is taking Indian cuisine in a bold new directionThis chef is taking Indian cuisine in a bold new direction
- Follow in the footsteps of Robin Hood in Sherwood ForestFollow in the footsteps of Robin Hood in Sherwood Forest